![Dalí, S. (1937). Sleep [oils on canvas]. Private collection.](https://www.research.colostate.edu/healthyagingcenter/wp-content/uploads/sites/32/2021/01/Dali-S..jpg)
Sleep
The average human spends over 24 years of life asleep, though the exact function of sleep remains a mystery. Sleep is not a behavior unique to humans. In fact, sleep-like behavior can be found across most species including organisms without centralized nervous systems like the box jellyfish (Cirelli & Tononi, 2008). Sleep is crucial for optimal cognitive and physical performance, health, and well-being, and unrelenting total sleep deprivation is fatal when implemented in rodents.
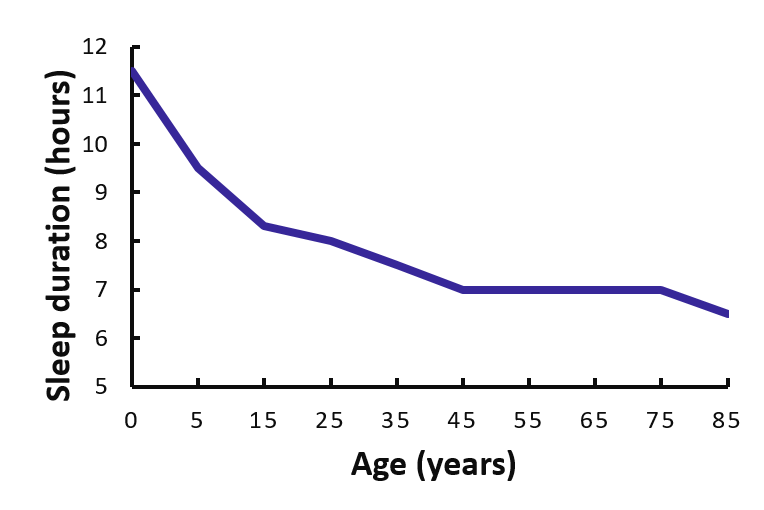
The American Academy of Sleep Medicine and the Sleep Research Society recommend adults sleep 7 or more hours each night on a regular basis to promote optimal health. Despite the universality and importance of sleep, there is a high prevalence of insufficient sleep in the modern world. The average sleep duration of American adults has decreased from ~8.8 hours to 6.8 hours over the last century (Redline et al., 2004; Tune, 1968) and 1 in 3 people report sleeping less than 6.5 hours per night during the work week. Behavioral sleep curtailment, normal aging, and sleep disorders like insomnia and sleep disordered breathing likely all contribute to this observed decline in sleep duration.
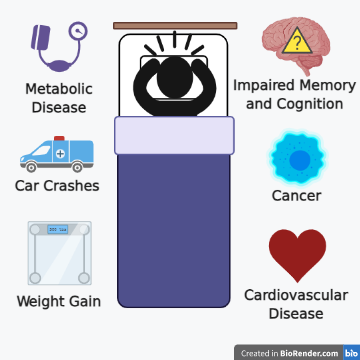
Insufficient sleep is associated with increased mortality rates and health problems. In fact, sleep disturbances, poor sleep quality, and short sleep duration all confer similar or higher risk for diabetes as being physically inactive (Anothaisintawee et al., 2016). Chronically insufficient sleep is also associated with increased risk for cardiovascular disease, cognitive decline, and impaired immune function.
Sleep and Heart Health
Insufficient sleep is associated with an increased risk for cardiovascular disease and a number of studies have reported elevated blood pressure during experimental sleep restriction. Elevated blood pressure is a risk factor for coronary heart disease, heart attacks, and stroke. For every hour that an adult typically sleeps less than 7 hours, there is an increase in coronary heart disease of 11% (Wang et al., 2016). If we extrapolate these finds to someone who typically sleeps 4 hours per night, their risk for coronary heart disease is 33% higher than if they were to sleep 7 hours per night.
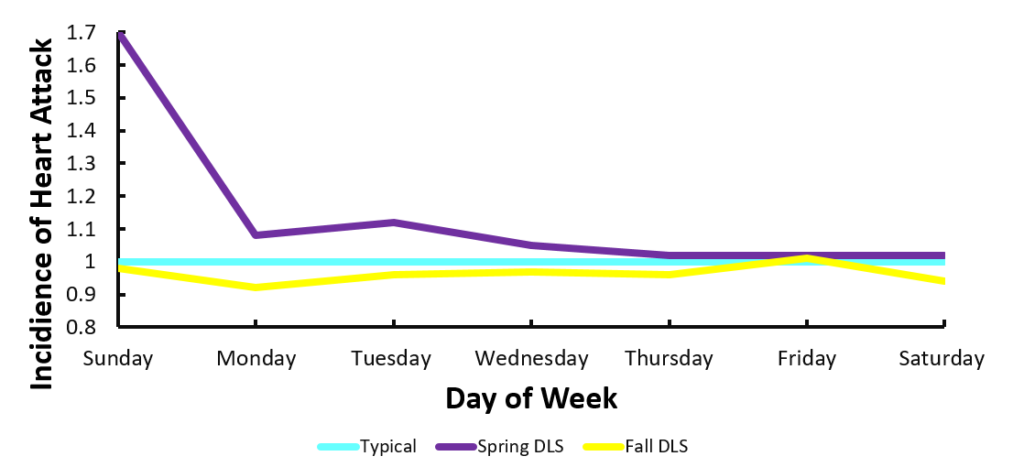
A situation that illustrates the relationship between sleep loss and heart attacks is daylight savings. Daylight savings time (DLS) in the Spring often induces acute sleep restriction, as most people lose an hour of sleep with the Springtime-change. Following this “spring forward,” there is a spike in heart attacks (Jiddou et al., 2013). Conversely, during the Fall when we set our clocks back, most people gain an hour of sleep, and subsequently the rate of heart attacks declines (Jiddou et al., 2013).
Sleep and Brain Health
Sleep is essential for optimal memory, learning, cognition, and mental health. Insufficient sleep is associated with an elevated risk for depression, dementia and Alzheimer’s disease, cognitive decline, and car crashes.
Chronic insufficient sleep and poor sleep quality are also associated with an heightened risk for depression, bipolar disorder, schizophrenia, and anxiety(Baglioni et al., 2016; Plante & Winkelman, 2008; Tsuno et al., 2005). Furthermore, for people diagnosed with aforementioned psychiatric disorders, sleep disturbances have been shown to exacerbates the severity of symptoms related to these disorders (Cox & Olatunji, 2016; Gruber et al., 2011). Sufficient sleep duration and quality may be an important therapeutic tool to minimize the risk for psychiatric disorders and limit the severity of symptoms in people diagnosed with psychiatric disorders.
Sleep deprivation can also impair learning and memory (Walker, 2009). In fact, pulling an all-nighter to prepare for an exam, a practice common amongst students, decreases the ability to learn and is linked to worse academic performance, measured my grade point average, compared to students who do not engage in pulling all-nighters (Thacher, 2008).
Insufficient sleep during midlife is also a risk factor for cognitive decline later in life and has been associated with an increased risk for Alzheimer’s Disease (Bubu et al., 2017; Virta et al., 2013). However, whether a causal link exists between insufficient sleep and Alzheimer’s Disease is not clear. Recent evidence does support that during insufficient sleep, there is a buildup of amyloid beta and tau, two toxic proteins that play important roles in Alzheimer’s Disease and may underpin disease progression (Holth et al., 2019; Shokri-Kojori et al., 2018).
Insufficient sleep is also linked to impaired motor skills, slower reaction time, and impaired driving ability. In an extensive traffic safety study conducted in 2016, the AAA Foundation in Washington D.C. examined over 7,000 drivers who had been involved in a car crash (Tefft, 2016). Drivers who had not received sufficient sleep in the 24 hours preluding the car crash, were more likely to be involved in car crashes and were significantly more likely to be at fault (Tefft, 2016). In fact, drivers who had gotten less than 5 hours of sleep were 3 times more likely to have a car crash. Drivers who had less than 4 hours of sleep the night before were 11.5 time more likely to be involved in a car crash. Based on the results from this analysis, authors reported that driving following a night of insufficient sleep is comparable to driving while legally drunk.
Sleep and Immune Health
Sleep is crucial for optimal immune health. Insufficient sleep increases susceptibility to viral infections such as the common cold (Prather et al., 2015) and is also associated with diminished effectiveness of vaccinations- specifically flue and hepatitis (Irwin, 2015; Prather et al., 2015).
Of note, the impact of insufficient sleep on susceptibility, severity, or risk of mortality due to COVID-19 infection are unknown. However, based on the relationship between insufficient sleep and viral infection susceptibility, it is possible that susceptibility to COVID-19 may be elevated during insufficient sleep. On the plus side, early evidence form a recent study reported that approximately half of Americans experienced improved sleep during the United States lockdown in response to COVID-19 (Gao & Scullin, 2020).
The reported reduction in natural killer cells associated with insufficient sleep has also been linked to heightened cancer risk. Specifically, people who typically sleep between 4 to 5 hours a night are at an 8% higher risk for dying of any type of cancers compared to people who typically sleep 7 or more hours per night (Li et al., 2019).
Sleep and Aging
Normal healthy aging is associated with changes in sleep quality and duration (Redline et al., 2004). Older adults have more nighttime awakenings, report shorter overall duration, as well as decreased deep sleep compared to younger adults. In fact, a reduction in deep sleep is apparent in people as young as 35 years of age. Older adults are also at a greater risk for sleep disorders such as insomnia and sleep apnea.
TIPS
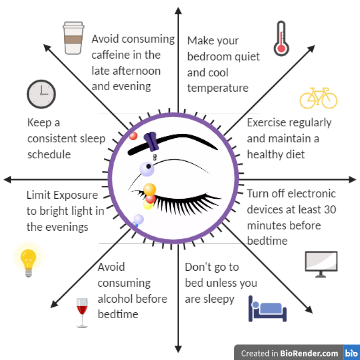
Establishing healthy sleep hygiene to optimize sleep duration and sleep quality can help individuals minimize the risk of disease, ranging from mental health, dementia and Alzheimer’s Disease, heart disease and obesity, and sickness like the flu and even some cancers. Below are suggestions for optimal sleep hygiene recommended by the American Academy of Sleep Medicine:
Takeaway
As we age, we are at an increasing risk for disease. Optimizing sleep duration and quality can promote healthy aging and may reduce disease risk associated with insufficient sleep.
Anothaisintawee, T., Reutrakul, S., Van Cauter, E., & Thakkinstian, A. (2016). Sleep disturbances compared to traditional risk factors for diabetes development: Systematic review and meta-analysis. Sleep Medicine Reviews, 30, 11–24. https://doi.org/10.1016/j.smrv.2015.10.002
Baglioni, C., Nanovska, S., Regen, W., Spiegelhalder, K., Feige, B., Nissen, C., Reynolds III, C. F., & Riemann, D. (2016). Sleep and mental disorders: A meta-analysis of polysomnographic research. Psychological Bulletin, 142(9), 969–990. https://doi.org/10.1037/bul0000053
Bubu, O. M., Brannick, M., Mortimer, J., Umasabor-Bubu, O., Sebastião, Y. V., Wen, Y., Schwartz, S., Borenstein, A. R., Wu, Y., Morgan, D., & Anderson, W. M. (2017). Sleep, cognitive impairment, and Alzheimer’s disease: A systematic review and meta-analysis. Sleep, 40(1). https://doi.org/10.1093/sleep/zsw032
Cirelli, C., & Tononi, G. (2008). Is sleep essential? PLOS Biology, 6(8), e216. https://doi.org/10.1371/journal.pbio.0060216
Cox, R. C., & Olatunji, B. O. (2016). A systematic review of sleep disturbance in anxiety and related disorders. Journal of Anxiety Disorders, 37, 104–129. https://doi.org/10.1016/j.janxdis.2015.12.001
Gao, C., & Scullin, M. K. (2020). Sleep health early in the coronavirus disease 2019 (COVID-19) outbreak in the United States: Integrating longitudinal, cross-sectional, and retrospective recall data. Sleep Medicine, 73, 1–10. https://doi.org/10.1016/j.sleep.2020.06.032
Gruber, J., Miklowitz, D. J., Harvey, A. G., Frank, E., Kupfer, D., Thase, M. E., Sachs, G. S., & Ketter, T. A. (2011). Sleep matters: Sleep functioning and course of illness in bipolar disorder. Journal of Affective Disorders, 134(1), 416–420. https://doi.org/10.1016/j.jad.2011.05.016
Holth, J. K., Fritschi, S. K., Wang, C., Pedersen, N. P., Cirrito, J. R., Mahan, T. E., Finn, M. B., Manis, M., Geerling, J. C., Fuller, P. M., Lucey, B. P., & Holtzman, D. M. (2019). The sleep-wake cycle regulates brain interstitial fluid tau in mice and CSF tau in humans. Science, 363(6429), 880–884. https://doi.org/10.1126/science.aav2546
Irwin, M. (2015). Why sleep is important for health: A psychoneuroimmunology perspective. Annual Review of Psychology. https://www.annualreviews.org/doi/full/10.1146/annurev-psych-010213-115205
Jiddou, M. R., Pica, M., Boura, J., Qu, L., & Franklin, B. A. (2013). Incidence of Myocardial Infarction With Shifts to and From Daylight Savings Time. The American Journal of Cardiology, 111(5), 631–635. https://doi.org/10.1016/j.amjcard.2012.11.010
Lee, Y. J., Cho, S.-J., Cho, I. H., & Kim, S. J. (2012). Insufficient sleep and suicidality in adolescents. Sleep, 35(4), 455–460. https://doi.org/10.5665/sleep.1722
Li, Y., Cai, S., Ling, Y., Mi, S., Fan, C., Zhong, Y., & Shen, Q. (2019). Association between total sleep time and all cancer mortality: Non-linear dose-response meta-analysis of cohort studies. Sleep Medicine, 60, 211–218. https://doi.org/10.1016/j.sleep.2019.03.026
Plante, D. T., & Winkelman, J. W. (2008). Sleep disturbance in bipolar eisorder: Therapeutic implications. American Journal of Psychiatry, 165(7), 830–843. https://doi.org/10.1176/appi.ajp.2008.08010077
Prather, A. A., Janicki-Deverts, D., Hall, M. H., & Cohen, S. (2015). Behaviorally assessed sleep and susceptibility to the common cold. Sleep, 38(9), 1353–1359. https://doi.org/10.5665/sleep.4968
Redline, S., Kirchner, H. L., Quan, S. F., Gottlieb, D. J., Kapur, V., & Newman, A. (2004). The effects of age, sex, ethnicity, and sleep-disordered breathing on sleep architecture. Archives of Internal Medicine, 164(4), 406. https://doi.org/10.1001/archinte.164.4.406
Shokri-Kojori, E., Wang, G.-J., Wiers, C. E., Demiral, S. B., Guo, M., Kim, S. W., Lindgren, E., Ramirez, V., Zehra, A., Freeman, C., Miller, G., Manza, P., Srivastava, T., Santi, S. D., Tomasi, D., Benveniste, H., & Volkow, N. D. (2018). β-Amyloid accumulation in the human brain after one night of sleep deprivation. Proceedings of the National Academy of Sciences, 115(17), 4483–4488. https://doi.org/10.1073/pnas.1721694115
Tefft, B. C. (2016). Acute sleep deprivation and risk of motor vehicle crash involvement. https://trid.trb.org/view/1436965
Thacher, P. V. (2008). University students and the “all nighter”: Correlates and patterns of students’ engagement in a single night of total sleep deprivation. Behavioral Sleep Medicine, 6(1), 16–31. https://doi.org/10.1080/15402000701796114
Tsuno, N., Besset, A., & Ritchie, K. (2005). Sleep and Depression. The Journal of Clinical Psychiatry, 66(10), 1254–1269. https://doi.org/10.4088/JCP.v66n1008
Tune, G. S. (1968). Sleep and wakefulness in normal human adults. British Medical Journal, 2(5600), 269–271.
Virta, J. J., Heikkilä, K., Perola, M., Koskenvuo, M., Räihä, I., Rinne, J. O., & Kaprio, J. (2013). Midlife sleep characteristics associated with late life cognitive function. Sleep, 36(10), 1533–1541. https://doi.org/10.5665/sleep.3052
Wang, D., Li, W., Cui, X., Meng, Y., Zhou, M., Xiao, L., Ma, J., Yi, G., & Chen, W. (2016). Sleep duration and risk of coronary heart disease: A systematic review and meta-analysis of prospective cohort studies. International Journal of Cardiology, 219, 231–239. https://doi.org/10.1016/j.ijcard.2016.06.027
About the Experts

Sophie Seward, M.S., is a doctoral student at Colorado State University. Her research is focused on the cardiovascular effects of sleep and circadian disruption.

Dr. Josiane Broussard is a clinical and translational scientist interested in sleep & circadian rhythms and metabolic health. She is an Assistant Professor in the Department of Health and Exercise Science at Colorado State University and the Division of Endocrinology, Metabolism and Diabetes and the University of Colorado Anschutz Medical Campus and directs the Sleep and Metabolism Laboratory at CSU. For the last 20 years she has been studying the mechanistic underpinnings of insulin resistance due to insufficient sleep and/or circadian misalignment, as well as potential countermeasures.








