
Blood Sugar (Glucose)
Blood sugar (blood glucose) control is critical to daily function. Muscles use sugar for energy every time we move, and as we age, two problems develop:
1 | Insulin Sensitivity
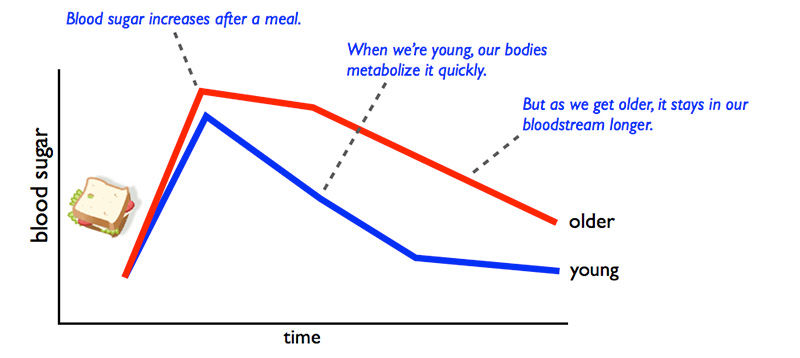
Young, healthy muscle and other tissues throughout the body are highly sensitive to insulin. Insulin helps cells use the glucose (sugar) that is circulating in the blood or stored in muscle. Insulin also controls how much fat is released from fat tissue into the bloodstream. However, as we age, our muscle and other tissues become less sensitive to insulin. This means that sugar (glucose) and fat (triglycerides) remain in the bloodstream longer, leading to poor blood sugar and blood lipid control.
2 | Insulin Production
After a meal, blood sugar rises, and a young pancreas produces insulin to stimulate uptake of that sugar into muscle and fat tissues throughout the body. This sugar is either used immediately for energy or stored for later use by exercising muscles. But as we age, the pancreas produces less insulin — which means blood sugar remains elevated for longer.
Why does this matter? Low insulin sensitivity and reduced insulin production can lead to poor control of blood sugars and fat, which can lead to diabetes. Diabetes can cause many complications including cardiovascular disease, stroke, chronic kidney failure and damage to the feet and eyes.
Tips:
So, what can you do? Many lifestyle strategies can prevent diabetes, including the following:
1 | Exercise Regularly
Research shows that even easy exercise increases insulin sensitivity in muscles and improves pancreas insulin production, which reduces your risk for many diseases including diabetes. Exercise, such as brisk walking, provides an immediate beneficial effect on insulin sensitivity and insulin production. In fact, exercise is more effective than most medications used to improve insulin sensitivity. Therefore, exercise is your best line of defense against diabetes.
- How much exercise should I do? The American Heart Association recommends 150 minutes per week of moderate aerobic exercise (like brisk walking) or 75 minutes of vigorous exercise (jogging, cycling, etc.).
- Does it matter when I exercise? While exercise any time of day is beneficial for blood glucose and triglycerides, some research suggests that the timing of exercise around a meal may be important. Aerobic exercise may have the most powerful effect when performed after a meal. This is likely because exercise slows the release of nutrients from the stomach and increases use of sugar by muscles. Interestingly, not only aerobic exercise but also resistance exercise — like lifting weights — can lower blood glucose and triglycerides following a meal. To sum up, both aerobic and resistance exercise following a meal would be good strategies to control your blood glucose and prevent diabetes.
- How hard should I exercise? Most research suggests that mild exercise such as brisk walking or lifting weights is enough to benefit insulin sensitivity and production — and the effect is immediate. However, it doesn’t last long. This means that you need at least a little exercise nearly every day to reduce the risk of diabetes. More vigorous exercise will improve your heart health and muscle strength. However, you should be careful when performing vigorous exercise to avoid developing low blood sugar (hypoglycemia). For the same reason that exercise is good for reducing blood sugar, there is a small chance that your blood sugar could drop too low with prolonged vigorous exercise. Blood sugar below 70 mg/dl can cause mental confusion, unconsciousness or seizures. Adding a little sugar — such as a sports energy drink mix — to your water bottle is a good idea for preventing too much of a drop in your blood sugar.
2 | Watch Your Sugar Intake
The average American eats 152 pounds of sugar per year!!! And, as we age, we lose our taste buds, which make us crave sugar more. Sugar is high in calories, and eating sugar leads to a spike in blood glucose. High consumption of sugar is linked to diabetes, and research also suggests that sugar is biologically addictive. As you eat sugar more, your brain craves more. So, watch your sugar intake!
In addition to exercise, eating less sugar is one of the best actions you can take to keep your blood sugar in the healthy range. Fructose, glucose, dextrose, lactose and maltodextrin are all types of sugar. Of these, fructose is especially harmful. Consumption of high-fructose-sweetened beverages (colas containing more than 50% high fructose corn syrup or sucrose) is associated with increased risk of cardiovascular disease and diabetes. So, read grocery labels carefully to know how much and what types of sugars you are eating. You can reduce your sugar intake by cutting down on candy, soda, sugary coffee drinks and sweet dessert at the end of every meal, processed or instant foods and salad dressing. Try replacing some of these things with fruit.
3 | Keep Your Waistline in Check
Approximately 70% of Americans are overweight, and being overweight increases your risk for developing diabetes. Most of us tend to put on weight around our mid-section as we age. The American Heart Association classifies a waistline greater than 40 inches for men, or 35 inches for women, as “high risk” for diabetes.
Why is body shape important? For years, researchers recognized that there was a strong connection between excess belly fat and diabetes or cardiovascular risk. In other words, apple-shaped people (those carrying fat in the abdomen) have a higher risk of diabetes and other diseases. On the other hand, our research group at the University of Colorado Anschutz Medical Campus was among the first to recognize that pear-shaped people (those carrying fat in the hips and thighs) seemed to be protected against risk of diabetes and cardiovascular disease. This is good news for people who tend to store their fat in the hips and thighs. However, for those of us who store our fat in the belly, keep exercising and watch that sugar intake!
About the Experts:

Rachael Van Pelt, Ph.D., is an Associate Professor of Medicine at the University of Colorado Anschutz Medical Campus. During the past 20 years, she has conducted research related to healthy aging, and much of her recent work has focused on insulin, glucose and lipid metabolism as it relates to cardiometabolic risk. Dr. Van Pelt’s research is supported by grants from the U.S. National Institutes of Health, and her laboratory provides training in aging research to post-graduate scientists.

Young-Min Park, Ph.D., is a Postdoctoral Fellow at the University of Colorado Anschutz Medical Campus. His research is focused on effects of physical activity and aerobic fitness on muscle insulin sensitivity and glucose control in aging adults.





