
Disparities in healthcare
The COVID-19 pandemic brought attention to several, massive health disparities that older adults in the United States face. The Center for Disease Control and Prevention defines health disparities as, “preventable differences in the burden of disease, injury, violence, or opportunities to achieve optimal health that are experienced by populations that have been disadvantaged by their social or economic status, geographic location, and environment.” Health disparities highlight inequities within the U.S. healthcare system, preventing some individuals from having a fair chance at accessing healthy living over others.
In particular, Black, Hispanic, American Indian, and Alaskan Native adult populations experience more infections, hospitalizations, and deaths from COVID-19, compared to white populations. More generally, racial and ethnic minority populations experience greater rates of poor health and disease, such as diabetes, hypertension, obesity, asthma, and heart disease. These trends can be tied back to a population’s socioeconomic status and its role in the types of healthcare they receive.
Dedicated research, a developing understanding of disparities, and societal change are needed to create intervention programs that promote health and longevity for all people, regardless of race, gender, identity, or socioeconomic status.
Health disparities research framework
The National Institute on Aging has created a framework to spearhead research on health disparities to address the different factors that contribute to inequalities and create intervention programs to promote health and well-being across the lifespan.
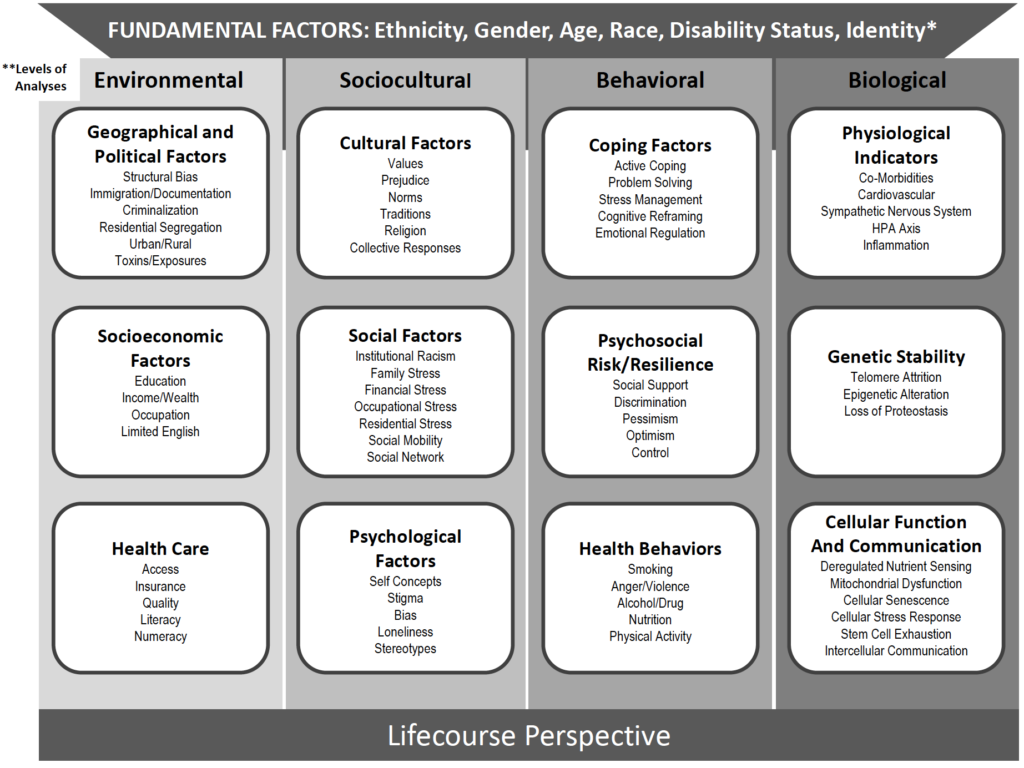
By conducting environmental, sociocultural, behavioral, and biological analyses within minority and racial populations, and understanding how these analyses intertwine with a host of micro-factors, health disparity researchers aim to identify why disparities emerge so that they can later resolve them.
Health inequities add up
To see how a health disparity is created, consider the example of particulate matter. These tiny, small particles pollute the air and can cause cellular damage that accelerates the aging process. Particulate matter comes from factories, power plants, transportation vehicles, and natural dust that lingers in the air.
Simply breathing these particles in can cause harm to individuals’ health. Studies have found that heavily populated Hispanic, African American, or low-income resident areas have more harmful particulate matter particles in the air. Due to the environmental and sociocultural status of the populations in these areas, their health is more at risk, despite harm being preventable. This is a health disparity.
To carry out the example even farther, individuals in these areas might be on Medicare, the health insurance of choice for most Americans in retirement. Our last blog established that the cost of Medicare is lofty for older adult populations. Many adults must make tradeoffs between basic goods like clothing, food, or over-the-counter drugs to pay for their healthcare needs.
Polluted air and healthcare spending aside, some adults may sacrifice a healthy diet to pay for their needed prescriptions. Being unable to afford nutritious foods falls into the NIA’s framework as a “behavioral factor” that could affect biology if an individual has a history of high blood pressure, cholesterol, or diabetes in their family. These are just a few examples of how one inequity can cascade into others, creating a health disparity for a larger group.
Diversifying population
Groups facing health disparities are only expected to grow in proportion in the U.S. Currently, 36% of the population belongs to racial or ethnic minority groups, and recent census data showed that the nation is diversifying faster than predicted.
These statistics make understanding health disparities of even more importance. Creating intervention programs that limit disparities is vital to ensuring that all individuals live healthier for longer.
ABOUT THE AUTHOR
Grace Weintrob is a senior majoring in Communication Studies with a minor in Stage, Sports, and Film Production at CSU. She is currently working as the digital media intern for the Columbine Health Systems Center for Healthy Aging.





